
Dysphagia: a tough diabetic pill to swallow
09 Feb 2023Chronic diabetes could trigger dysphagia, a swallowing disorder that could severely limit food and fluid intake
Diabetic neuropathy (nerve damage due to diabetes) could trigger an array of complications. One such disorder is difficulty swallowing. Commonly known as dysphagia, this condition can affect the quality of life of a person as it may limit food intake and even take away the joy of savouring food. The damaged nerves affect the contracting ability of the muscles along the esophagus (food pipe) making it difficult to push ingested food down to the stomach.
“It is important for the swallowing muscles to be working in the throat to push the food to the right pathway rather than the windpipe,” explains Dr S Phaneedhar Reddy, consultant, speech-language pathologist, feeding and swallowing specialist, Apollo Hospitals, Jubilee Hills, Hyderabad.
Diabetes and dysphagia
The food reaches the stomach smoothly when the esophagus muscles are intact. These muscles could be affected by a nervous system disorder, stroke or even cancerous growths. People with chronic diabetes are at a higher risk of dysphagia because they are more susceptible to diabetic neuropathy, a disorder of the nervous system.
Dysphagia can be of two types – oropharyngeal and esophageal. While oropharyngeal dysphagia can affect the nerves of the mouth and throat, in esophageal dysphagia the muscles of the food pipe are damaged and don’t work in pushing the food down.
“With no movement in the throat or the food pipe, it is difficult to swallow and propel the food into the stomach,” elaborates Dr Manjunath Malige, lead consultant, endocrinology and diabetes, Aster RV Hospital, Bengaluru.
Fungal infections like oseophageal candidiasis which will progress into oseophageal dysphagia are also triggers in people with diabetes, mainly because of their compromised immune system.
Dr Malige explains that in diabetics, dysphagia is often accompanied by high-risk co-morbidities like end-stage organ damage and comorbidities like hypertension and obesity with a high risk for stroke and heart attacks.
Dysphagia symptoms
Symptoms of dysphagia include:
- Nausea
- Vomiting
- Abdominal discomfort
- Diarrhea
“All these are manifestations of nerve damage due to diabetes,” explains Dr S M Fayaz, consultant, internal medicine, diabetology, Kinder Women’s Hospital and Fertility Centre, Bengaluru.
“The usual complaint of a diabetic with dysphagia is that they cough every time they eat and try to swallow food,” explains Dr Malige. They might even experience a sticky feeling in the throat even after not having eaten anything.
“Diabetes can also lead to esophageal motility disorders (EMD) that cause swallowing difficulties, spasms of pain and acid reflux,” adds Dr Fayaz. The swallowing difficulties due to EMD is also a major cause of dysphagia.
Complications
Dysphagia may lead to complications like malnutrition, dehydration, aspiration pneumonia (if the food or liquid gets into the airways or lungs) and other pulmonary complications. If not attended to in time, the infection may spread into the bloodstream and affect the lungs by forming abscesses.
Treatment
Dr. H K Susheen Dutt, senior consultant and ENT specialist, Fortis Hospital, Bengaluru, explains the three key ways to manage dysphagia. They include incorporating swallowing therapy, dietary changes and using feeding tubes in people with eating and swallowing difficulties.
The initial stage of dysphagia is treated by a gastroenterologist with nausea and vomiting-reducing medication. However, if the person doesn’t respond to the medical line of management, then a surgically fitted gastric pacemaker can help send electrical impulses to stimulate the stomach after eating.
In some cases, these people might require hospitalisation with IV fluids and injections. Once they start taking food, the injections are replaced with tablets. While recovery time varies from person to person, if there is neurological damage then the condition can be lifelong. Qualified speech therapists and swallowing therapists can help people with dysphagia by teaching them
Diabetes dysphagia case study
Dr Reddy recalls a recent case of a 55-year-old male with diabetes who had stroke-induced dysphagia. This person was being tube fed for one month because he was unable to eat and swallow which also led to fluctuations in his sugar levels.
Dr Reddy and his team decided to improve muscular coordination with a swallowing strategy and therapy. Within five days of the treatment, the dysphagia-affected person started swallowing two to three ml of liquids every day under Dr Reddy’s supervision. Within fifteen days, he was able to consume more food without a feeding tube.
Although his condition was not extremely severe, it took the person fifteen days to recuperate. But in severe cases, this condition may get more challenging, explains Dr Reddy.
“If this doesn’t work, the person may be asked to switch to a nasogastric tube which goes from the nose into the stomach to make sure the nutrition is taken care of,” adds Dr. H K Susheen Dutt
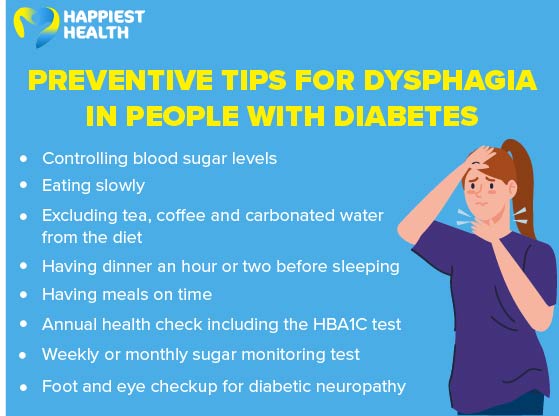
Takeaways
Long-lasting and uncontrolled sugar levels can damage the oral and esophageal nerves due to dysphagia. This can make eating and swallowing a complex process and could prevent people with diabetes from getting adequate nourishment.

